Introduction
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder affecting reproductive-aged women. It is characterized by ovulatory dysfunction, hyperandrogenism, and polycystic ovaries.
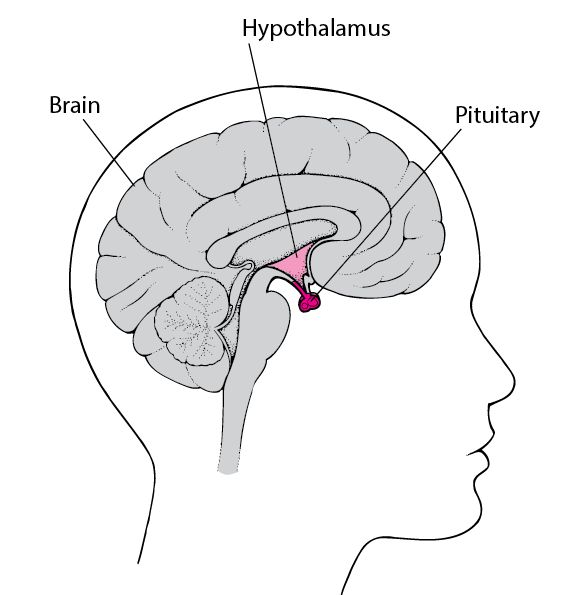
Pathophysiology of PCOS
- Insulin resistance → Hyperinsulinemia → Increased androgen production.
- Excess androgens → Hirsutism, acne, menstrual irregularities.
- Ovarian dysfunction → Anovulation, infertility, polycystic ovaries.
Clinical Features
- Menstrual irregularities (Oligomenorrhea, amenorrhea).
- Hirsutism & acne due to excess androgens.
- Obesity & insulin resistance (Increased diabetes risk).
- Infertility & increased risk of endometrial cancer.
Diagnosis
-
Rotterdam Criteria (Two out of three required):
- Oligo-ovulation or anovulation.
- Clinical/biochemical signs of hyperandrogenism.
- Polycystic ovaries on ultrasound.
Management
- Lifestyle modifications (Weight loss, exercise).
- Oral contraceptive pills (OCPs) for menstrual regulation.
- Metformin for insulin resistance.
- Clomiphene citrate or Letrozole for infertility.
Conclusion
PCOS requires a multidisciplinary approach involving lifestyle changes, hormonal therapy, and fertility treatments. These MBBS notes are essential for understanding PCOS management.